For Healthcare Professionals
STOP to consider
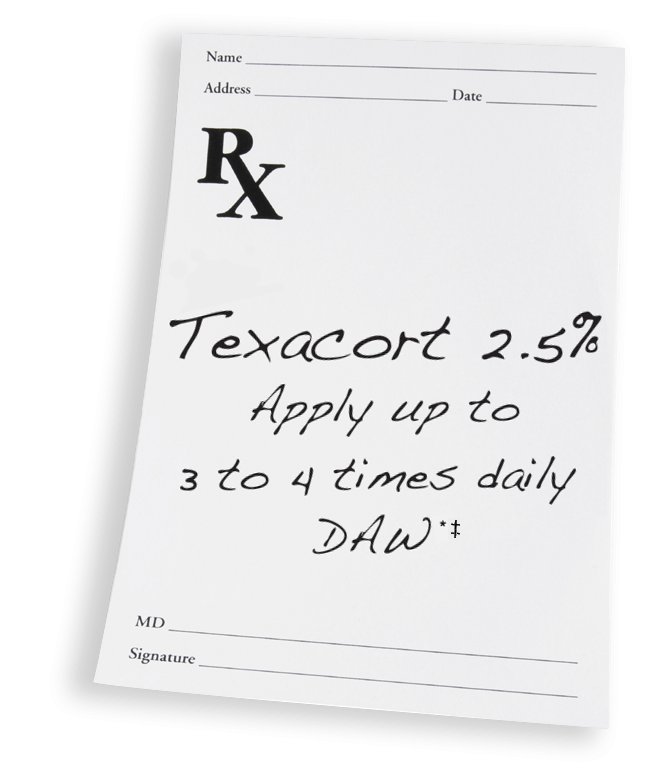
The only 2.5% hydrocortisone steroid solution available*
DROP to provide a clear topical solution
Class 7, low-potency corticosteroid with specially designed dosing applicator
GO with added features and benefits
Developed for patient adaptability
*FDA Orange Book, December 2023.
†To be used for illustrative purposes only. Individual dose will vary by patient and condition.
‡Use language required by state: D.A.W. (dispense as written), B.M.N. (brand medically necessary), or D.N.S. (do not substitute).